What is schizophrenia?
Schizophrenia is a complex mental health condition that affects how a person thinks, feels, and behaves. It is often described as a form of psychosis, defined as losing some contact with reality or experiencing reality in a very different way to those around them. This may be through symptoms such as audio or visual hallucinations, and delusions.
The term schizophrenia is taken from the Latin words “schizo” - to split - and “phrene” - the mind, which can lead to confusion around its symptoms. However, patients with schizophrenia do not have a split personality. Instead, they may experience a wide range of symptoms, including:
- Hallucinations - seeing or hearing things that aren’t really there
- Delusions - beliefs that are not based on reality
- Muddled thoughts and speech that may be based on hallucinations or delusions
- Feeling disconnected from your feelings and emotions
- Disorganised thinking and behaviour
- Not wanting to look after your personal needs
- Wanting to avoid people, including friends and family
What causes schizophrenia?
The cause of schizophrenia is not fully understood; however, many experts believe it is linked to a combination of genetic and environmental factors. For example, schizophrenia has been seen to run in families and a number of different genes may increase a person’s risk of developing the condition.
A person’s environment and life experiences may also play a role in the development of schizophrenia. This can include living in poverty or exposure to stressful or dangerous environments. Exposure to viruses or nutritional problems before birth may also be linked to the condition.
There is some evidence to suggest that people with schizophrenia may be more likely to have differences in the size of certain brain areas and connections between brain areas; however, more research is needed to better understand how brain structure and function may relate to the condition.
Schizophrenia and quality of life
The complexity of schizophrenia means that it can often affect all areas of a person’s life, including personal endeavours, relationships, and educational and occupational functioning. Furthermore, individuals with schizophrenia often face stigma and discrimination.
The World Health Organisation (WHO) also acknowledges that individuals with schizophrenia often experience human rights violations “both inside mental health institutions and in community settings.” These factors mean that people with the condition may face social exclusion which can limit their access to general health care, education, housing, and employment.
What are the treatments for schizophrenia?
Schizophrenia can be a lifelong diagnosis. This means that treatment focuses on regaining a good quality of life instead of “curing” the condition. Common interventions include a combination of medicine and therapies tailored to each individual. This can include:
- Antipsychotic medicines - including typical and atypical antipsychotics
- Cognitive behavioural therapy (CBT)
- Support from a community mental health team (CMHT)
If schizophrenia is well managed, the risk of relapse can be greatly diminished. Many patients with the condition will go on to recover completely without experiencing another episode. Unfortunately, the vast majority of people with schizophrenia around the world are not receiving mental health care.
Furthermore, some medications for schizophrenia may have negative side effects. For example, side effects of typical antipsychotics can include muscle twitches and spasms, shaking, and trembling. Side effects of both typical and atypical antipsychotics can include drowsiness, weight gain, blurred vision, and lack of sex drive. This can lead some patients to discontinue their medication, putting them at risk of relapse.
Schizophrenia and cannabis
Several studies have linked cannabis use with an increased risk of developing psychotic disorders, including schizophrenia. As the authors of one study point out, heavy cannabis users are over-represented among new cases of schizophrenia. There has therefore been much debate on this topic with research aiming to better understand this apparent relationship.
Some suggest that cannabis use may contribute to psychosis in some individuals. A recent study, published in Psychological Medicine concluded that young men with cannabis use disorder have an increased risk of developing schizophrenia. The authors estimated that as high as 30% of cases of schizophrenia among men aged 21-30 may have been prevented by averting cannabis use disorder. However, these findings assume a causal relationship between cannabis use and schizophrenia.
On the other hand, others suggest that patients who are vulnerable to developing schizophrenia and other psychotic conditions may simply be more likely to self-medicate with cannabis. But no matter the relationship between cannabis use and schizophrenia, it is generally advised that patients with a history of psychosis avoid the drug - particularly THC (the main psychoactive component of cannabis).

Graham Woodward, a former NHS psychiatric nurse and Releaf COO, notes:
“Legacy cannabis has historically been linked to psychosis, potentially due to the high THC levels found in strains like Super Skunk. Additionally, recreational or ‘legacy cannabis’ often contains contaminants such as pesticides and growth enhancers, and there have been instances of legacy cannabis being sprayed with substances like Spice.
“Another critical factor to consider is the hereditary predisposition for developing psychosis or schizophrenia. Genetic factors can increase the risk of these conditions, making the use of cannabis particularly concerning for these individuals.”
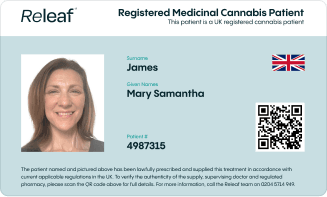
Medical cannabis in patients with schizophrenia
Medical cannabis can be useful in the treatment of a number of conditions. Some medical cannabis formulations may be beneficial for certain mental health problems, including anxiety, which can be a major symptom of schizophrenia. However, a thorough patient assessment should always be conducted before recommending or prescribing medical cannabis. As Mr Woodward explains:
“Although medical cannabis has been shown to benefit other mental health symptoms such as anxiety and depression, the current evidence available does not support its application in patients with schizophrenia due to the numerous risks involved.
“Our primary responsibility is to keep patients safe and improve their health outcomes. Therefore, until more conclusive evidence is available, we must err on the side of caution and prioritise proven safe and effective treatments for this vulnerable population."
Final thoughts
There is still much to learn regarding cannabis use and the development of schizophrenia. While a causal relationship between the drug and psychosis has not been proven, it is important to recognise the potential risks associated with the use of cannabis in some patient populations, including those with a history of schizophrenia. Thorough patient screening and assessment of medical history are essential in the safe and responsible prescribing of cannabis-based medicines.